Research | October 2018 Hearing Review
Hearing care professionals often encounter people who complain of hearing difficulties and trouble hearing in noise, but when tested, present with hearing sensitivity and thresholds that are within “normal limits.” This article reviews the audiological evidence regarding this unique population and makes the case for educating them about sophisticated technology options—including hearing aids and wireless technology such as remote microphones—which have been proven to be extremely useful for enhancing their communication and quality of life.
Approximately 38 million people in the United States have hearing loss.1 The inability to understand speech-in-noise (SIN) is one of the main complaints of people with untreated sensorineural hearing loss (SNHL), as well as many people who wear traditional hearing aids.2 It is also estimated that an additional 26 million American adults possess hearing thresholds within the range of normal limits (WNL), but they, too, complain of hearing difficulty (HD) and SIN problems, as will be reviewed below.
These additional 26 million adults with HD and/or SIN problems (ie, suprathreshold auditory deficits) often report experiencing a reduced quality of life (QOL) due to their auditory problems (see sidebar, “A Common Scenario”). When these individuals seek help from audiologists, they are often informed that their hearing thresholds are WNL and are subsequently counseled about advantages that can be derived from better lighting, use of visual redundancy, sitting closer to the person speaking, and other advice given to persons with hearing loss in traditional auditory rehabilitation programs. However, it is likely that many of these individuals are not being tested thoroughly or that traditional audiometric tests are not sensitive enough to determine their actual SIN ability. It is also likely that these people are not being informed of commercially available tools that could improve the signal-to-noise ratio (SNR), and, thus, address their listening and communication needs and potentially lead to positive benefits. Indeed, Tremblay and colleagues3 asked why people with normal hearing sensitivity (ie, pure-tone thresholds WNLs) still complain of HDs and/or trouble understanding SIN.
This article reviews published benefits that are associated with improving the SNR for some adults and children who present with hearing sensitivity and thresholds which are generally accepted as within normal limits (WNL) but have HD and/or trouble understanding SIN. We also review and speculate on benefits that some people receive from enhanced SNRs which are delivered through sophisticated hearing aids and remote microphone (RM) systems, and technologies that can be wirelessly coupled to personal hearing aids and other devices.
Demographics
Tremblay and colleagues3 reported that 12% of adults with normal hearing report having HD. They reviewed research associated with complaints of HD despite hearing thresholds WNL, which included:
- Saunders and Haggard4 found that 29% of older adults who passed pure-tone tests self-reported a hearing handicap.
- Gates and colleagues5 reported that 20% of the 683 people in the Framingham Study self-reported hearing loss yet had normal pure-tone sensitivity.
- Chia and colleagues6 reported that 51% of their subjects (49+ years of age) reported HD, yet only half of those had hearing loss based on standard audiometry.
- Spankovich and colleagues7 examined the report of HD among adult participants of the National Health and Nutrition Examination Survey (NHANES), an ongoing cross-sectional survey that is generalizable to the US civilian non-institutionalized population. They reported that 10-15% of those who presented WNL also reported HD.
- Jacobson8 reported that some individuals with suspected hearing loss based on self-reports of difficulty with speech recognition and trouble understanding SIN also presented as WNL.
The present population of the United States is estimated to be about 327 million people9; approximately 250 million are adults over 18 years of age and 85 million are children. If 38 million have hearing loss, then about 289 million people in the United States have normal hearing, and perhaps 75% of those, or 217 million, are adults. If about 12% of adults who present with hearing WNL also have HD and/or trouble understanding SIN, then some 26 million US adults may exhibit these problems.
Scope of the Problem
Assuming that 26 million adults have HD and/or trouble understanding SIN despite hearing thresholds WNL and that about 38 million people have demonstrable (audiogram-based) hearing loss, then the potential population of those within the United States with HD may be 64 million people. As such, one of the most important roles of audiologists is to identify people who might benefit from medical, surgical, or amplification intervention and refer appropriately. This standard applies in all cases, but it is becoming increasingly important for adults who present with hearing thresholds WNL and ambiguous symptoms.
A Common Scenario
Mrs Smith, a 35-year-old wife and mother of three children and head of a small business, is Dr Jones’ first patient of the day. Dr Jones has been an audiologist for over 30 years. He greets Mrs Smith, walks her into his office, and begins to take a case history. He notices that Mrs Smith seems to have slight difficulty answering his questions and she seems somewhat stressed.
Mrs Smith reveals that she has been having increasing difficulty hearing her husband and children at home and her employees at weekly staff meetings. She reports difficulty hearing friends in noisy restaurants and prefers to not go to movies anymore because she cannot follow conversations, especially when people have accents, and she says the background sounds and music are way too loud.
Her case history is relatively benign. She denied having previous otologic conditions or medications. Mrs Smith did report some noise exposure with shotguns and tractors when she was younger on the farm in Iowa and while working for a few years in a noisy printing factory. Her major complaints included some hearing difficulties (HDs) and trouble understanding speech in noise (SIN), as well as occasional tinnitus and hyperacusis.
Dr Jones has seen many patients with these complaints over the years and expects to find that she has a mild-to-moderate sensorineural hearing loss. However, after completing his routine diagnostic audiometric tests, he found that her hearing was within normal limits; the low- and mid-frequency pure-tone thresholds were 5-10 dB HL and those above 2000 Hz were at 25 dB HL. The only abnormal findings were slightly poorer-than-normal results on the SIN test and decreased otoacoustic emissions at the higher frequencies.
The diagnosis was not what Mrs. Smith expected and seemed to cause her even more concern as she began to question her sanity. Having seen many cases like this over his career, Dr Jones reassured her that he believed her complaints were real and that she was neither crazy nor a hypochondriac. Fortunately, Dr Jones was aware of current research on patients with similar problems. He briefly informed her about hidden hearing loss (HHL) and cochlear synaptopathy (CS) and related auditory disorders, suggesting there could be a connection with her symptoms.
Rather than simply sending her on her way with a recommendation to be re-tested in a year, or sooner if things got worse, Dr Jones informed her about some technologies which might offer solutions to her problems. She began a trial with mild-gain, advanced digital technology hearing aids and he set her up with a remote microphone (RM) for use in meetings and at restaurants.
She returned the next week. Dr Jones expected that Mrs Smith would return the hearing aids and RM due to the slight nature of her hearing loss, as few people want to wear hearing aids if they do not have to. But he was surprised to find that Mrs Smith reported that she was hearing much better at home and at work and that the RM had functioned well on two occasions during the previous week. She further reported that she had worn the hearing aids for about 8 hours a day and that her tinnitus was not nearly as bothersome when wearing the aids, and that, although loud sounds still bothered her, they were more tolerable with the hearing aids. She stated that she was less stressed when wearing the hearing aids and that she did not have to try so hard to hear with them; listening seemed to require less effort.
Indeed, these improvements were reflected on the pre and post self-report questionnaires that Dr Jones had Mrs Smith complete. Thus, Mrs Smith received positive solutions and outcomes for her HDs. It is likely that most hearing care professionals have encountered patients with similar scenarios. This increasingly common scenario should remind clinicians that it is important to listen to their patients’ complaints and be ready to help them find solutions for their HDs.
Validated self-report assessment tools can help identify the extent of these HDs from the perspective of the patient. For example, although originally designed to assess listening and communication status quo and needs for people with hearing loss, instruments like the Client Oriented Scale of Improvement (COSI), the Hearing Handicap Inventory for Adults (HHIA), and similar assessment tools can be adapted for use with people who have hearing sensitivity WNL yet present with HD and/or SIN problems. Hannula and colleagues10 found that self-reported HDs are more frequent (37% for HDs and 43% for following a conversation in noise) than hearing loss as defined by persons’ audiometric thresholds. Jerger11 indicated that there are more dimensions to hearing impairment and hearing handicap than hearing loss alone.
Although many clinicians use self-assessment scales like the COSI or HHIA for hearing aid candidates, they may not regularly employ them to assess people who present WNL. The Abbreviated Profile of Hearing Aid Benefit (APHAB) is a standardized self-reporting tool that assesses hearing problems in daily life through a 24-item questionnaire.12 The APHAB examines speech communication in different environments including favorable, reverberant, and noisy conditions to create a global score that reflects overall communication problems. The APHAB has considerable normative data, which makes it easy to compare individuals’ findings to expected performance. The HHIA consists of 25-items (13 emotional and 12 social-situational), has been standardized on adults, and scores range from no perceived handicap to a significant perceived hearing handicap.13 The Personal Assessment of Communication Abilities (PACA) is a 12-item self-report questionnaire that has been validated on adults with normal and near-normal hearing which can help identify and prioritize areas of communication improvement in adults with possible SIN challenges.14
People who present with hearing WNL but have supra-threshold auditory deficits are not uncommon. Multiple terms have been used to describe these deficits including: central presbycusis, auditory disability with normal hearing, obscure auditory dysfunction (OAD), King-Kopetzky Syndrome, auditory dysacusis, central auditory processing disorder (CAPD) or auditory processing disorder (APD), idiopathic discriminatory dysfunction, hidden hearing loss (HHL), cochlear synaptopathy (CS), and HDs, among others. Of note, people with auditory abnormalities (eg, auditory neuropathy spectrum disorder (ANSD), CS, and APD may present with overlapping or similar signs and symptoms of HD and/or SIN problems.15
Normal Hearing
Defining “normal hearing” is a challenge, and several published definitions are available. For example, the American Speech-Language-Hearing Association16 defines degrees of hearing and hearing loss as:
- Normal (-15 dB to +15 dB HL),
- Slight (16-25 dB HL),
- Mild (26-40 dB HL),
- Moderate (41-55 dB HL),
- Moderately severe (56-70 dB HL),
- Severe (71-90 dB HL), and
- Profound (91 dB HL+).
Pienkowski17 reported that peripheral auditory nervous system (PANS) deficits can exist even with 0 dB HL thresholds. He stated that PANS deficits are probable between 10-20 dB HL. Pienkowski reported that the average pure-tone thresholds of healthy young adults when measured in quiet are 0 dB HL and cited evidence that standard deviations range from 3-5 dB between 100 Hz and 8000 Hz. The standard deviation widens to 10 dB at roughly 14-16 kHz. He concluded that the 95% confidence intervals (CIs, in this case, 95% probability that the dB HL values would fall within this range) for healthy young adults would be ±10 dB (ie, ranging from -10 to +10 dB HL) through 8000 Hz. Interestingly, he noted that defining normal hearing as up to and including 20 dB HL (from 100 to 8000 Hz) was dubious at best.
Spankovich and Le Prell18 and Spankovich and colleagues7 noted that perceived hearing loss in the presence of normal audiometric thresholds may be related to several factors. They also suggested that the definition of normal hearing is not as simple as some would like. Most epidemiological reports use the four-frequency pure-tone average (4FPTA at 500, 1000, 2000, and 4000 Hz); however, some formulas substitute 3000 Hz for 4000 Hz, and others specify that if the inter-octave thresholds are 20 dB or greater, then inter-octave mid-frequency tones (ie, 750, 1500, 3000, and 6000 Hz) should be included in the 4FPTA.
The term “normal hearing,” as applied to audiometric data, literally refers to pure-tone threshold sensitivity of 0 dB HL. The American National Standards Institute (ANSI) defines 0 dB HL as normal-hearing threshold sensitivity based on research defining Reference Equivalent Threshold Sensitivity, or Sound Pressure Level (RETSPL). Unfortunately, textbooks and multiple national professional organizations refer to normal hearing (sensitivity) as being between 0 and 25 dB HL, which gives the impression that patients with thresholds in this range have no auditory disorder—based on audibility. However, a threshold of 5 dB HL represents a deviation from “normal hearing” of 5 dB and one can argue that thresholds in the 20-25 dB HL range represent a significant deviation from normal and could be additional justification for the provision of advanced technology for improved speech recognition.
We believe that it is incorrect to refer to those with threshold sensitivity in the 5-25 dB HL range as having “normal” hearing…It would be helpful and more appropriate for patients to have their complaints of hearing difficulties taken more seriously if the audiology profession would adopt a phrase like “hearing sensitivity within the range of normal limits.”
The arbitrariness of threshold-based definitions of hearing loss is further complicated by the fact that the definition of “normal” changes with age. We believe that it is incorrect to refer to those with threshold sensitivity in the 5-25 dB HL range as having “normal” hearing. Indeed, the fact that individual listeners with similar audiometric thresholds can exhibit a wide range of HD and/or SIN problems has been reported for decades.19,20 It would be helpful and more appropriate for patients to have their complaints of HDs taken more seriously if the audiology profession would adopt a phrase like “hearing sensitivity within the range of normal limits” when describing such audiometric configurations.
Possible Etiologies
Hidden hearing loss and cochlear synaptopathy. Barbee et al21 stated that standard audiometric evaluations are not sensitive enough to identity people with HHL or CS. Johnson et al22 noted that people who have trouble understanding SIN often express frustration when audiologists use standard hearing threshold measures and advise patients that their hearing sensitivity is “normal.”
The existence of HD despite hearing thresholds WNL can be related to several peripheral and central etiologies. HHL23 refers to reduced neural output from the cochlea as described by Kujawa and Liberman24 who demonstrated that noise, aging, and exposure to ototoxic drugs can cause substantial insults to synaptic elements without overt changes to thresholds. Kujawa and Liberman25 stated that inner hair cell and auditory nerve fiber synapses are the most vulnerable parts of the ear to noise exposure. This type of pathology is thought of as “hidden” because it is often not reflected by change in pure-tone thresholds, and hair cells may remain intact which makes assessing synaptic integrity and survival of the spiral ganglion difficult, despite loss of synapses. A marker commonly used to measure synaptopathy is a reduction in auditory brainstem response (ABR) Wave-I amplitude.26 CS refers to primary synapse damage,24 while the term HHL has been used to refer generically to functional deficits (eg, HD and/or trouble understanding SIN) in the presence of hearing WNL.
The correlation between CS and perceptual deficits in humans is presently speculative. Lobarinas and colleagues27 provided evidence of changes in animals’ ability to detect signals in multiple SNRs resulting in a sustained decrease in ABR Wave-I amplitude with recovered thresholds and otoacoustic emissions. However, the work in humans has been inconclusive, with some studies suggesting relationships to peripheral auditory evoked potentials (AEPs) and others showing no relationship.7 The susceptibility of humans to CS as result of noise exposure, aging, and ototoxic drugs remains unclear. Spankovich and Le Prell18 reported the presence of CS secondary to aging and noise exposure, which may influence SIN performance across various listening situations.
Extensive case histories and an appropriately modified test battery may help identify these patients, particularly those with prior exposure to noise and/or ototoxic agents, which could place them at risk for CS. For example, Liberman and colleagues28 investigated a potential test battery on young musicians at high risk for CS and non-musician peers who were at low risk for CS. The high-risk group had significantly poorer high-frequency thresholds above 8000 Hz and poorer SIN with temporal distortion (ie, time compression and reverberation), and greater summating-to-action potential ratios than those in the low-risk group.
Many of these patients also complain of tinnitus. For example, Bramhall and colleagues26 found an association between reduced amplitude of ABR Wave-I and tinnitus in veterans and non-veterans and concluded that tinnitus may be a common symptom in patients with CS. These potential associations are being investigated further and research should shed light on these connections soon.
In the not-too-distant future, it may be possible for persons at risk for HD caused by excessive noise exposure to be administered pharmacotherapeutic agents and/or otoprotective compounds to prevent or perhaps reverse CS and/or noise-induced hearing loss. Pre-clinical studies using animal models have shown the effectiveness of certain compounds in protecting the cochlea against noise exposure.29 Translating promising results from pre-clinical animal studies to clinical use with humans will require the development of a test battery for CS that can be used in Phase II clinical trials and that can be adapted for routine use in audiology clinics to help make earlier diagnoses of these problems than is possible with the current battery. A goal of such trials would be that HDs experienced by patients with CS and/or HHL may be able to be prevented, diagnosed earlier, and/or treated more effectively.
Extended high-frequency hearing loss. Spankovich and Le Prell18 noted that large population-based studies of hearing thresholds extending beyond 8000 Hz have not been performed. However, smaller data sets are available and there is evidence that elevated extended high-frequency thresholds can contribute to SIN difficulty30 which may indicate potential CS at apical (lower frequency) regions of the cochlea.31 Basal (higher frequency) regions of the cochlea are more susceptible to acquired hearing loss and should be included in the assessment of individuals reporting HD.3,7 Conflicting results have been reported in studies that have investigated extended high-frequency hearing loss. For example, Bramhall and colleagues26 found no significant differences between high-frequency thresholds in veterans and non-veterans with and without histories of noise exposure. However, Liberman and colleagues28 found significantly poorer high-frequency thresholds in young musicians compared to those of their non-musician peers. Interestingly, Prendergast and colleagues32 found that the greater the histories of noise exposure, the poorer were the high-frequency thresholds of females (but not of males).
Auditory processing disorders (APD). The terms CAPD or APD are highly controversial in the contemporary audiology literature.33 Indeed, Jerger34 argued that APD means different things to different people. Regardless of one’s stance on this concept, one of the primary symptoms of APD is difficulty processing SIN, and test batteries for APD typically include a SIN measure, which makes it relevant to this article.
The mainstream APD concept was explained on The Ohio State University website35 which stated that APDs are disorders in which people appear to have peripheral hearing loss yet have hearing WNL on an audiogram. Clearly, APDs are not a simple or single condition, and unfortunately, there is no conclusive consensus among professionals regarding the definition of APD, let alone how to diagnose or treat APD.
Kricos36 reviewed the effects of aging on auditory processing and changes in the central auditory system that may affect everyday listening situations for people with hearing thresholds WNL. She reported that older individuals with hearing thresholds WNL may experience cognitive, intellectual, attention, and processing difficulties. Moore37 suggested that APD in children may represent a listening difficulty (LiD) which may involve more than a disorder in the auditory system. In children with HDs, there appears to be more of a neuropsychological and psychophysiological development issue which combines language, learning, and cognition. Tremblay and colleagues3 concluded that some adults have HD despite hearing thresholds WNL, which has been described by multiple terms as discussed above. These terms have been used inconsistently in the literature, and the sources and etiology of these HDs remain unclear.
Beck et al38 reported that APD may overlap with language impairment, dyslexia, attention deficit disorder (ADD), attention deficit hyperactivity disorder (AD/HD), as well as ANSD, CS, and more. Dillon39 defined spatial processing disorders as a specific form of APD and reported that some children with normal-hearing thresholds and generally normal intelligibility in quiet and noise are not able to use acoustic spatial cues to separate speech from noise which affects their ability to focus their attention properly and may result in a diagnosis of APD.
Management of APDs often includes the use of assistive devices to improve the SNRs in classrooms, homes, and places of work. Although personal or sound field FM systems were most often used in the past, remote microphones (RMs) with hearing aids are now the preferred technology.
Management of APDs often includes the use of assistive devices to improve the SNRs in classrooms, homes, and places of work. Although personal or sound field FM systems were most often used in the past, remote microphones (RMs) with hearing aids are now the preferred technology. Keith and Purdy40 reported on the beneficial effects of amplification using RMs that include improving the SNR and having a therapeutic effect.
Auditory neuropathy spectrum disorder (ANSD). ANSD was first described in 1996 by Starr and colleagues41 as a hearing disorder characterized by an absent or grossly abnormal ABR, cochlear function as indicated by present otoacoustic emissions (OAEs) and/or cochlear microphonic, and absent middle-ear muscle reflexes. The underlying pathology of ANSD is assumed to be a dyssynchronous firing of the auditory nerve fibers, which leads to grossly abnormal resolution of the temporal components of speech and reduced speech intelligibility.42,43 The term auditory neuropathy was subsequently updated to a spectrum disorder given the wide variation in the auditory function of patients with ANSD, many of whom present with audiograms WNL or profound SNHL.
Clearly, the audiogram does not always predict auditory function, and the perceptual consequences vary dramatically. In children with congenital ANSD, acquisition of spoken language is almost always delayed, and intervention is hampered by the lack of objective tests to predict benefit from personal amplification.
Rance and colleagues44 described 20 patients with confirmed ANSD who underwent a battery of tests including: pure-tone and speech audiometry, ABR, OAEs, and steady-state evoked potentials. Pure-tone audiometry showed normal three-frequency (500, 1000, and 2000 Hz) pure-tone averages (PTAs) in 8 of 38 ears. The authors reported that although some patients used hearing aids successfully, their benefit was more limited than in patients with SNHL.45 Cochlear implants (CIs) have provided significant benefit in some people with ANSD when peripheral and central auditory nervous systems are intact.45-47
Assistive listening technology (eg, FM systems) is universally recommended for people with ANSD as they require an improved SNR relative to people presenting WNL or with cochlear hearing loss. ANSD may be an acquired condition. For example, Yuvaraj and Jayaram48 found 38 adolescents and adults (16-30 years of age) with confirmed late-onset ANSD that ranged from 9-29 years. The ANSD was of sudden onset in 9 patients and demonstrated a gradual progression of increasing HD in the remaining 29 patients.
Other possible etiologies. An exhaustive listing of all possible etiologies for HD and/or trouble understanding SIN given hearing WNL is beyond the scope of this article. However, some etiologies include: aging, dementia, cognitive decline, presbycusis (originating from sensory, neural, synaptic, auditory fiber, and/or central causes), noise-induced hearing loss (NIHL), traumatic brain injury (TBI), mild cognitive impairment (MCI), receptive aphasia, neurocognitive disorders, and Alzheimer’s Disease, among others.49
Speech-in-Noise Tests
Understanding speech in noise has long been a primary complaint of people with mild-to-moderate sensorineural hearing loss, even though many have been fitted with traditional hearing aid amplification systems. Although the American Academy of Audiology (AAA) and the American Speech-Language-Hearing Association (ASHA) have each published best practice (BP) statements recommending use of SIN tests as a necessary part of comprehensive adult audiologic evaluations, fewer than 15% of audiologists appear to perform SIN tests routinely on their patients.50 Clark and colleagues51 found that only 15% of the audiologist respondents in their study said they used pre-treatment, self-assessment measures; 10% used post-fitting validation outcome questionnaires; and 15% used SIN tests regularly.
Several SIN tests have been available for decades. For adults, common SIN tests include the adult versions of the Bamford-Kowal-Bench Speech-in-Noise test (BKB-SIN),52,53 the Words-in-Noise Test (WIN),54 the Hearing in Noise Test (HINT),55 and the QuickSIN,56 among others, which have been shown to have high validity and test reliability. According to Schafter,57 SIN tests for the pediatric population include the BKB-SIN for children 5 years of age and older,58 the Hearing in Noise Test for Children (HINT-C)59 for children 6-12 years of age, and the Pediatric Speech Intelligibility (PSI) test60 for children 3-6 years of age. The AZbio test is available for children 8 years of age and older and the Babybio is available for children 6-8 years of age.61,62
Some SIN tests (eg, HINT and QuickSIN) are adaptive, where the level of the speech or the noise increases or decreases depending upon the patient’s performance, typically converging on a proportion correct rate of 50%. Other measures such as the Connected Speech Test (CST)63 and the Speech Perception in Noise (SPIN)64 tests use fixed speech and noise levels.
It is not clear whether an “ideal” SIN test should have fixed or adaptive SNR levels or whether the speech material should be natural sentences, spondees, or monosyllabic words, but a multi-talker babble using four or more talkers should be used as the competing background sound. Other commonly used competing stimuli include pink, speech spectrum, and white noise, but they are not ideal options as they do not contain linguistic information and acoustic fine-structure found in competing speech. Artificial noises may be easier for listeners to ignore than are natural human-produced speech sounds.65 Moreover, the use of a noise competitor in addition to temporal distortion from time compression and reverberation may result in speech recognition tasks that could help identify patients with HDs. For example, as indicated earlier, Liberman and colleagues28 found significantly poorer word recognition scores for SNRs of 0 and +5 dB and time compression with and without reverberation by young musicians at high risk for CS than by their low-risk, non-musician peers.
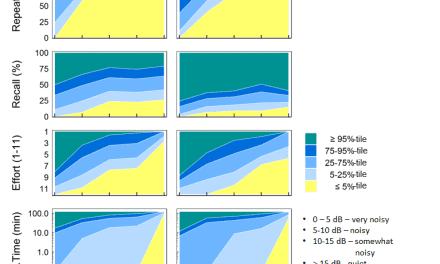
Wilson66 reported on the speech recognition in noise ability of 3,024 adult veterans of the US military using the WIN. This large sample ranged in age in whole decades between 20 and 80 years, and average high-frequency pure-tone averages ranged between 15-70 dB HL. Presentation levels were louder than conversational speech to minimize the influence of reduced audibility for participants with hearing loss. Among the factors investigated, age and pure-tone average were the strongest predictors of speech recognition in noise ability, with high-frequency pure-tone average being the strongest predictor. One hallmark of these data was the variance in performance that was seen when parsing the data by age and pure-tone average. Although older participants and those with more hearing loss showed the greatest variance, those younger and with less hearing also showed sufficient variance to be meaningful clinically. This inter-individual variance and the lack of wholly predictive utility in the factors of age and severity of hearing loss motivated Wilson to recommend including the assessment of speech recognition in noise ability as part of every audiologic diagnostic assessment.
Considerations of speech recognition in noise ability should not stop at performance measurements alone. Individuals’ subjective judgments of their own speech recognition ability or the effort they must expend to function during routine, but challenging, conversation may provide complementary insight to support counseling of patients who report hearing difficulties that would not be predicted by their age or hearing sensitivity.
Considerations of speech recognition in noise ability should not stop at performance measurements alone. Individuals’ subjective judgments of their own speech recognition ability or the effort they must expend to function during routine, but challenging, conversation may provide complementary insight to support counseling of patients who report hearing difficulties that would not be predicted by their age or hearing sensitivity. Indeed, patients’ own perceived ratings of listening effort expended during speech recognition tasks may assist audiologists in identifying persons with HD and SIN problems. Listening effort has been defined as the mental effort needed to understand speech or other signals.67,68 Johnson and colleagues69 found that patients could use a simple, single-item listening scale to rate their own perceived listening effort during the completion of a speech recognition task. However, more research is needed to identify a standard SIN test and measure of listening effort with normative date for persons without HD before establishing performance criteria necessary for making a clinical diagnosis of HD.
Benefits of an Improved SNR
In the last decade several studies have highlighted the benefits of improving the SNR for listeners with both normal hearing and those with hearing loss. The emergence of user-friendly wireless technology has improved the ability to understand SIN without the need for cumbersome, corded, body-worn systems.
Thibodeau and Schaper70 suggested that wireless technology tools may allow users to approach SIN results that were obtained by people with relatively normal hearing ability. Technology options for people with hearing challenges include sophisticated devices worn at or completely in the ear. In educational and many conversational situations, a RM is worn by the person speaking, from which the signal is wirelessly transmitted to a receiver worn by the listener directly into the hearing aids or to a classroom speaker system. The placement of a RM near the mouth of the speaker results in improved SNRs and speech recognition in noise.
Johnson and colleagues71 reported on two groups of children with normal hearing. Ten children were in an experimental group (average age = 12 years); all of these children were diagnosed with APDs and fitted with non-occluding, ear-level style FM receiver systems for school use and they were encouraged to use the FM system at home. Thirteen children served as the control group (average age = 11 years); none of these children were diagnosed with APDs, and except for acquiring an FM system baseline measure, they were not fitted with FM systems. The authors reported that compared to the age- and gender-matched control group, the baseline FM measures for the children with APD were significantly lower for speech perception scores, and the experimental group displayed decreased academic performance and had more psychosocial problems. However, measures for the experimental group during the school year with FM systems demonstrated speech perception improvement in noisy classrooms and significant benefits were found in academic and psychosocial arenas. After 5 months of FM use by the children with APD, parent and student ratings improved regarding focus-of-control, anxiety, depression, and interpersonal relationships.
Kuk and colleagues72 noted in 2008 that children with APD often have SNR difficulty, yet at the time their paper was published personal amplification systems were not widely offered as a solution to the SNR problem. Their study was designed to determine whether personal hearing aid amplification systems might improve SIN performance for attentiveness, speech recognition, and daily functioning in 14 children (7-11 years of age) who were diagnosed with APD. Each child wore open-ear, mild-gain, behind-the-ear, wide-dynamic range compression hearing aids adjusted to provide approximately 10 dB of insertion gain for conversational input. Directional microphone and noise-reduction systems were engaged. The children were encouraged to wear their amplification system at school, home, and during social activities, and they were evaluated at their initial visit/fitting, as well as at 2 weeks, 3 months, and 6 months post-fitting. The Northwestern University word-list (NU-6), Auditory Continuous Performance Test (ACPT), and the Children’s Auditory Processing Performance Scale (CHAPS) questionnaires were the primary assessment tools. The SIN results for omnidirectional microphone were essentially the same as unaided. However, noise reduction in tandem with directional microphones did improve speech understanding in noise. Although the amplification systems evaluated in 2008 reduced the number of errors on the ACPT and improved several areas on the CHAPS, the authors reported that their results were not statistically significant. The authors also indicated that sophisticated open-ear fitting hearing aids could be attempted on some children with APD.
Adults also benefit from improved SNRs resulting from use of wireless technology. Thibodeau and DeConde Johnson reported that increased use of wireless technology by people with hearing challenges outside of educational settings were apparent and not limited to those with hearing loss.
Adults also benefit from improved SNRs resulting from use of wireless technology. Thibodeau and DeConde Johnson73 reported that increased use of wireless technology by people with hearing challenges outside of educational settings were apparent and not limited to those with hearing loss. Further, evidence shows that adults with TBIs, particularly veterans, benefit from improved SNRs while using RMs. Saunders and colleagues74 reported that audiologists who are increasingly addressing the needs of blast-exposed veterans who present with hearing WNL yet have HD, or problems with SIN. They suggested that clinicians should consider SIN ability, listening and communication demands, auditory lifestyle, possible post-traumatic stress disorder (PTSD), and other mental health factors, and that education of the patients, spouses, and families is critical to successful outcomes. Gallun et al75 and Beck et al49 also described successful use of FM systems by veterans. In particular, they reported that when audiologists worked with patients having experienced blast exposure and normal or near-normal audiograms, hearing aid fittings were also successful.
Saunders and colleagues76 reported that many blast-exposed veterans complained of trouble understanding SIN and rapid speech, and difficulty following instructions. These HDs are often considered to be disproportionate to patients’ peripheral hearing sensitivity. The authors concluded that FM and RM systems using Bluetooth are effective interventions for blast-exposed veterans with normal or near-normal hearing sensitivity, but functional HDs and these tools should routinely be considered as an intervention approach. The benefits of mild amplification and use of RMs is not limited to veterans. Smart et al77 reported positive benefits from using mild-gain hearing aid fittings with FM and RMs in adults with APD.
Beck et al49 reported that people with neurocognitive disorders and TBIs often experience significant advantages from amplification systems which reduce background noise and improve SNRs. They reported that sophisticated hearing aids maintain more realistic and naturally occurring spatial cues which allow wearers to know where to focus their attention. Providing spatial information through personal amplification systems allows hearing aid wearers to compare unique signals from the left and the right ears, similar to how people with hearing thresholds WNL know where to attend. The authors reported that these advantages enhance QOL and may soon serve a neuroprotective role against cognitive decline that is associated with hearing loss and some neurocognitive disorders.
Improving SNRs can be achieved using several technologies, and methods presently available appear to achieve similar results. Galster and Rodemerk78 investigated four commercially available RM systems, each with a different wireless transmission protocol (FM, 900 MHz, 2.4 GHz, or Bluetooth). A total of 16 adults (52-81 years of age) with mild to moderately severe hearing loss served as subjects and the HINT was used as the measurement tool. The authors reported that all of the RM systems statistically significantly improved SIN outcomes when compared to unaided scores, and when compared to those obtained in noise while using hearing aids without RMs. The benefits received via the four RMs were comparable to those observed with traditional FMs.
Well-Fitted Hearing Aids, SIN, and HD
In a double-blind study, Valente and colleagues79 investigated differences in word and sentence recognition in quiet and noise, as well as responses to two subjective questionnaires in 24 new hearing aid users. Participants wore and were tested with binaural hearing aids fit to the manufacturer’s “first-fit” algorithm versus fitting the hearing aids to NAL-NL2 targets using probe-tube measures (ie, “matched”). At the end of the study, 19 of the 24 participants preferred the matched response (probe-tube measure). Also, improvements in word recognition at input levels of 50 and 65 dB SPL were significantly better for the matched response.
As early as 1975, Winchester80 noted that all persons with hearing disorders were hearing aid candidates and that it was inaccurate to think that certain types of HDs could not benefit from properly fitted hearing aids. Indeed, fitting hearing aids to patients based on their perceived HDs is not a new concept. Bennett81 evaluated hearing aid use by patients with hearing threshold levels of 20 dB or better at 500 and 1000 Hz, and 35 dB or better at 2000 Hz. Of 98 patients who completed a 30-day trial with hearing aids, 92% elected to purchase the aids and 85% considered their hearing aids to be a worthwhile investment after 6 months of use.
Beck and Le Goff82 compared word recognition scores and improvements in SNRs for 25 adults (73 years of age) who wore three different hearing aid technologies. The participants were tested while three different talkers spoke randomly and while noise originated from three locations. The participants’ task was to repeat test words while wearing directional, narrow-band directional (beam-forming), and multi-speaker access technology (MSAT) devices. All three technologies improved the SNR. Across all listening tasks, the directional technology improved the average speech reception threshold required to achieve 50% correct (SRT-50) by 4.9 dB, the narrow-band directionality improved it by 5.5 dB, and the MSAT improved it by 6.3 dB. As SRT-50s improved from directional to narrow-band directional, an overall improvement in WRS of +7% was reported, and from narrow-band directionality to MSAT, an additional 11% improvement in WRS was noted. The improvements in word recognition scores and in SNRs were shown to be statistically significant.
The results indicate that mild-gain amplification is a viable treatment option for some individuals who present with hearing difficulty, but whose thresholds are within normal limits.
Roup et al15 described results for two groups of adults with normal-hearing sensitivity. Participants included 20 normal-hearing adults (19-27 years of age) with no self-reported HDs, and 19 normal-hearing adults (18-58 years of age) with self-reported HDs. The HD group was fitted binaurally with mild-gain, receiver-in-the-canal (RIC) hearing aids for a 4-week trial with directional and noise-reduction algorithms engaged. The hearing aids were verified to provide 5-10 dB of insertion gain between 1000 and 4000 Hz. Assessment tools included the HHIA and the Auditory Processing Questionnaire (APQ) and auditory processing abilities were assessed using the SCAN-3:A, the Dichotic Digits Test (DDT), the Gaps-in-Noise (GIN)test, and a 500 Hz Masking Level Difference (MLD) task. The SIN measures were acquired pre and post hearing aid fitting. The authors reported that 67% of those fitted stated that the hearing aids helped a little or a lot in quiet, and 71% stated that the hearing aids helped a little or a lot in noise. The results indicated that mild-gain amplification is a viable treatment option for some individuals who present with HD, but whose hearing thresholds are WNL.
Remote Microphone (RM) Systems
RM systems are radio devices that contain a RM (eg, lapel, tabletop, or boom microphones) that captures the audio signal of interest and delivers it via radio frequency (RF) transmission to a radio receiver that is coupled to the listener’s hearing aids. RM systems improve speech recognition in noise by improving the SNR, reducing reverberation, and minimizing the deleterious effects of distance on sound.83,84 Wolfe and colleagues85 reported that when using RM systems, children with hearing loss achieved better speech recognition in noise than children and adults with normal hearing at SNRs commonly encountered in real-world listening environments (eg, -5 to +5 dB SNR) .
Historically, most RM systems transmitted the audio signal from a microphone to radio receivers via a frequency modulated (FM) radio signal. Today, however, most RM systems deliver the audio signal from the microphone to radio receivers via digital RF transmission. Digital RF transmission provides several advantages over FM transmission including: an essential elimination of the potential for interference from other nearby RF systems, a reduction in the noise and static that occasionally accompanied FM signals, a wider audio bandwidth, and an increase in the sophistication of processing that may be applied to the transmitted signal. Indeed, research has shown conclusively that superior speech recognition in noise is possible with the use of digital RF systems relative to FM systems.86,87
Digital RM systems are available in two broad forms: universal personal RM systems and accessory RM systems. Universal personal RM systems contain receivers that are designed to be coupled to hearing aids of most major manufacturers (eg, special adapters are available to allow for connection of the universal RF receiver to almost any make and model of modern hearing aids). The primary advantage of a universal RM system is that one RM can deliver an audio signal to multiple listeners who may be using different makes and models of hearing aids (eg, several children with hearing loss in a classroom may receive an audio signal from a single RM).
Accessory RMs are typically designed to operate only with the hearing aids of the manufacturer that has developed the RM system. Accessory RM systems are typically less expensive than universal personal FM systems. All major hearing aid manufacturers now offer relatively inexpensive digital RM systems that transmit audio signals via digital RF from a RM to a radio receiver integrated within the body of the hearing aid. Alternatively, some accessory RM systems deliver the audio signal to an RF receiver worn on the listener’s body. Then, the audio signal is transmitted from the body-worn receiver to the hearing aid via near-field magnetic induction (NFMI).
Accessory RM technology has improved considerably over the past several years and many accessory RM systems include features such as digital noise reduction, directional microphones to reduce surrounding noise and improve the SNR, and accelerometers to detect the orientation of the microphone and to select the most appropriate microphone mode (eg, directional or omnidirectional) automatically. Unfortunately, there is a paucity of research examining performance differences obtained with universal personal RM systems versus accessory RM systems.88 However, research examining the potential benefits of accessory RM systems has shown average improvements in speech recognition in noise of 60% or more relative to the no RM condition at SNRs commonly encountered in real-world situations (eg, 0-5 dB SNR).88-90 Given these findings, accessory RM systems are exceptionally effective for improving speech recognition in noise, and audiologists should strongly consider recommending RM technology for individuals who are experiencing difficulty understanding SIN.
[Keith and Purdy] indicated that remote microphones offer a range of therapeutic benefits including: improved cortical auditory-evoked potentials (CAEPs), ABRs, frequency discrimination, binaural temporal resolution, frequency pattern recognition, and auditory working memory, among others. Assistive benefits include: improved attention, learning, behavior, participation in class, self-esteem, and psychosocial development.
Keith and Purdy40 noted that digital RM hearing aids are hybrid radio and hearing aid systems that may be helpful for children with normal peripheral hearing. They indicated that FM systems are being replaced by RM systems and that the latter have performed very well for people with APD, dyslexia, autism spectrum disorder, and attention and other learning disorders. The authors indicated that RMs offer a range of therapeutic benefits including: improved cortical auditory-evoked potentials (CAEPs), ABRs, frequency discrimination, binaural temporal resolution, frequency pattern recognition, and auditory working memory, among others. Assistive benefits include: improved attention, learning, behavior, participation in class, self-esteem, and psychosocial development. Some RMs offer up to 15-20 dB improvement in SNR, and hearing aids with personal RMs are presently the only evidence-based amplification treatment option that has been shown to improve hearing in classrooms for children with APD by overcoming acoustic barriers and providing auditory access in classrooms.
Schafer and colleagues91 reported that RM technology—including FM and/or digital transmission (DT)—is a form of hearing assistive technology (HAT) that may be used to increase, maintain, and improve the functional abilities of children. The authors provided evidence that RM HAT systems significantly improve behavioral performance and subjective listening ability for appropriate children. They concluded that audiologists can improve auditory performance via RM HAT for children with reduced SIN ability, problematic auditory processing, reduced classroom performance, and listening difficulties.
Salehi et al92 reported that hearing aids with directional mics are the most common solution to SNR problems and that they offer 2-3 dB of SNR benefit in typical fittings. However, the SNR benefit decreases as noise and reverberation increase. They reported that in the most deleterious listening situations, RMs can significantly enhance listening by offering an increase in the SNR of up to 20 dB. They stated that contemporary RMs use digital wireless communication strategies and incorporate digital signal processing (DSP) algorithms. Therefore, RMs can provide substantial benefit to hearing-impaired persons, even in acoustically challenging listening environments with noise and reverberation.
In addition, modern RMs have been shown to benefit CI patients as well. Fitzpatrick and colleagues93 reported on 15 adult CI users who combined RMs with their CIs. They stated that these CI participants demonstrated improved speech understanding while watching television news and talk shows and using RMs with their CIs. These CI users reported that the RM gave them more confidence, better comprehension, and greater ease of listening than when using the CI without the RM. Additionally, Wolfe and colleagues87,89 have shown that CI recipients typically experience 40-70% improvements in SIN with the use of RM systems at SNRs commonly encountered in realistic environments (eg, 0-10 dB SNR). Again, use of RM systems is the most effective way to improve speech recognition in noise.
Discussion
In addition to the nearly 38 million people in the United States with documented hearing loss, there are potentially an additional 26 million adults with HD and/or trouble understanding SIN, despite having hearing WNLs. Beck and Flexer94 stated that hearing is perceiving sound, whereas listening is the ability to make sense of or derive meaning from sound, and that listening is where hearing meets brain. As we learn more about HD, HHL and CS, trouble understanding SIN, hyperacusis, and tinnitus, it is increasingly apparent that many of these auditory disorders and symptoms overlap.
The ability to listen in challenging acoustic environments involves much more than simply having hearing WNL as measured by the traditional pure-tone audiogram. Because listening involves the ability to make sense of sounds that are perceived in quiet environments and within noisy and reverberant backgrounds, “normal hearing” goes beyond the auditory system and involves decoding, attention, memory, language skills, and working memory, and it can be adversely impacted by the effects of noise exposure, cognitive ability, and aging. Further, it seems apparent that audiologic testing should include aided and unaided sound-field tests at quiet and normal conversational levels, with and without competing speech babble.
Although some contemporary sophisticated hearing aids have been shown to improve the SNR by 6 dB or more,82 significantly greater SNR improvements can be achieved with telecoils, FM systems, and wireless RMs. In addition to mild-gain, high-tech hearing aids, these technologies should be introduced and demonstrated to patients who complain of HDs and SIN difficulty, but who have normal or near-normal audiometric thresholds.
Comprehensive audiometric tests beyond routine audiometrics must be conducted based on the context of patients’ self-reported complaints. Person-centered care dictates that we engage in a treatment decisionmaking process that encompasses the components of evidence-based practice based upon available research, expert opinion, and a demonstrated appreciation for patients’ expressed experiences, needs, and concerns. Unfortunately, tests in the traditional audiometric battery are not sensitive enough to pick up and validate many patients’ complaints.
Comprehensive audiometric tests beyond routine audiometrics must be conducted based on the context of patients’ self-reported complaints. Person-centered care dictates that we engage in a treatment decisionmaking process that encompasses the components of evidence-based practice based upon available research, expert opinion, and a demonstrated appreciation for patients’ expressed experiences, needs, and concerns.95 Unfortunately, tests in the traditional audiometric battery are not sensitive enough to pick up and validate many patients’ complaints. Several researchers are working to develop a modified test battery to that end.22
Some patients with auditory complaints and hearing thresholds WNL may decline treatment and be satisfied with the simple knowledge and reassurance that their HDs are real and not just perceived. Others may want to explore treatment options and solutions that could include communication management discussions and training as well as investigation of potential benefits that may be derived through modern hearing aids and sound management technologies. In applying the latter treatment option, audiologists must proceed with caution, assess potential benefits of contemporary solutions on a trial basis, and use pre- and post-treatment measures to determine if patients experience positive outcomes and reductions of their self-reported HDs and audiometric complaints.
Final Thoughts
Almost everyone hears better and is more relaxed in a quiet environment. Unfortunately, noise is ubiquitous. Almost everyone perceives and appreciates high-fidelity auditory sounds when the acoustic information is received at favorable SNRs. Many adults and children actually require and prefer enhanced SNRs and need facilitative access to auditory information in order to converse, learn, and participate in professional, social, recreational, and academic situations.
Or, as questioned by Roup, are audiologists doing a disservice to patients who seek their care, when they label their hearing as normal or mild, despite complaints and supra-threshold auditory deficits in the presence of hearing within normal limits as determined by traditional audiometric tests?
Audiologists must ask themselves, “Am I offering information, hearing aid trials, SNR-enhancing technologies, and services that may enhance the QOL of all my patients, including those with slight or mild hearing losses and/or complaints of HDs and trouble understanding SIN?” Or, as questioned by Roup,96 are audiologists doing a disservice to patients who seek their care, when they label their hearing as normal or mild, despite complaints and supra-threshold auditory deficits in the presence of hearing WNL as determined by traditional audiometric tests?
Audiologists are the experts in hearing assessment and management. Patients, adults, and children alike need to know that they can count on their audiologists to identify and treat their problems and expand their access to auditory experiences competently, compassionately, and professionally. Beck et al49 stated that improving the brain’s ability to listen (ie, derive meaning from sound) through technologies that can improve the SNR may enhance individuals’ QOL and may soon even prove to serve a neuroprotective role against cognitive decline associated with hearing loss and neurocognitive disorders.
References
-
Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. 2016;106(10)1820-1822.
-
Abrams HB, Kihm J. An introduction to MarkeTrak IX: A new baseline for the hearing aid market. Hearing Review. 2015;22(6):16.
-
Tremblay KL, Pinto A, Fischer ME, et al. Self-reported hearing difficulties among adults with normal audiograms: The Beaver Dam Offspring Study. Ear Hear. 2015;36(6): e290-299.
-
Saunders GH, Haggard MP. The clinical assessment of obscure auditory dysfunction—1. Auditory and psychological factors. Ear Hear. 1989;10(3):200-208.
-
Gates GA, Cooper JC, Kannel WB, Miller NJ. Hearing in the elderly: The Framingham cohort, 1983-1985. Part 1. Basic audiometric test results. Basic audiometric test results. Ear Hear. 1990;11(4):247-256.
-
Chia E-M, Wang JJ, Rochtchina E, Cumming. RR, Newall P, Mitchell P. Hearing impairment and health-related quality of life: The Blue Mountains Hearing Study. Ear Hear. 200;28(2):187-195.
-
Spankovich C, Gonzalez VB, Su D, Bishop CE. Self-reported hearing difficulty, tinnitus, and normal audiometric thresholds, The National Health and Nutrition Examination Survey 1999-2002. Hear Res. 2018;358:30-36.
-
Jacobson G. Hearing difficulties in the absence of hearing loss. J Am Acad Audiol. 2018;29(6):456. DOI: https://doi.org/10.3766/jaaa.29.6.1
-
US Population 2018. Worldometers website. Available at: http://www.worldometers.info/world-population/us-population/
-
Hannula S, Bloigu R, Majamaa K, Sorri M, Mäki-Torkko E. Self-reported hearing problems among older adults: Prevalence and comparison to measured hearing impairment. J Am Acad Audiol. 2011;22(8):550-559.
-
Jerger J. Why do people without hearing loss have hearing complaints? J Am Acad Audiol. 2011;22(8):490.
-
Johnson JA, Cox RM, Alexander GC. Development of APHAB norms for WDRC hearing aids and comparisons with original norms. Ear Hear. 2010;31(1):47-55.
-
Newman CW, Hug GA, Jacobson GP, Sandridge SA. Perceived hearing handicap of patients with unilateral or mild hearing loss. Ann Oto Rhino Larngol. 1997;106(3):210-214.
-
Taylor B, Manchaiah V, Clutterbuck S. Using the Personal Assessment of Communication Abilities (PACA) tool. Hearing Review. 2016;23(3):20.
-
Roup CM, Post E, Lewis, J. Mild-gain hearing aids as a treatment for adults with self-reported hearing difficulties. J Am Acad Audiol. 2018;29(6):477-494.
-
American Speech-Language-Hearing Association (ASHA). Type, degree, and configuration of hearing loss [PDF]. 2015. Available at: https://www.asha.org/uploadedFiles/AIS-Hearing-Loss-Types-Degree-Configuration.pdf
-
Pienkowski M. On the etiology of listening difficulties in noise despite clinically normal audiograms. Ear Hear. 2017;38(2):135-148.
-
Spankovich C, Le Prell C. Perspectives on: “Normal” hearing and perceived hearing complaints. Audiology Today. 2017;29(6):34-44.
-
Olsen WO, Tillman, TW. Hearing aids and sensorineural hearing loss. Ann Otol, Rhinol, Laryngol. 1968;77(4):717-726.
-
Dubno JR, Dirks DD, Morgan DE. Effects of age and mild hearing loss on speech recognition in noise. J Am Acad Audiol. 1984;76(1):87.
-
Barbee CM, James JA, Park JH, et al. Effectiveness of auditory measures for detecting hidden hearing loss and/or cochlear synaptopathy: A systematic review. Seminars Hear. 2018;39(2):172-209.
-
Johnson CE, Barbee CM, Danhauer JL, Jilla AM, Kimball SH, Seever KL. Toward the future of early intervention for adult hearing loss. Seminars Hear. 2018;39(2):221-226.
-
Schaette R, McAlpine D. Tinnitus with a normal audiogram: Physiological evidence for hidden hearing loss and computational model. J Neurosci. 2011;31(38):13452-13457.
-
Kujawa SG, Liberman MC. Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci. 2009;29(45):14077-14085.
-
Kujawa S, Liberman MC. Hidden hearing loss—The problem and the promise. Association for Research in Otolaryngology. Available at: https://www.aro.org/page/KujawaLiberman
-
Bramhall NF, Konrad-Martin D, McMillan GP, Griest, SE. Auditory brainstem response altered in humans with noise exposure despite normal outer hair cell function. Ear Hear. 2017;38(1):e1-e12.
-
Lobarinas E, Spankovich C, Le Prell CG. Evidence of “hidden hearing loss” following noise exposures that produce robust TTS and ABR wave-I amplitude reductions. Hear Res. 2017;349:155-163.
-
Liberman MC, Epstein MJ, Cleveland SS, Wang H, Maison SF. Toward a differential diagnosis of hidden hearing loss in humans. PLOS One. 2016;11(9):e0162726
-
Choi C-H, Du X, Floyd RA, Kopke, RD. Therapeutic effects of orally administrated antioxidant drugs on acute noise-induced hearing loss. Free Radical Research. 2014;48(3):264-272.
-
Badri R, Siegel JH, Wright BA. Auditory filter shapes and high-frequency hearing in adults who have impaired speech in noise performance despite clinically normal audiograms. J Acoust Soc Am. 2011;129(2):852.
-
Fernandez KA, Jeffers PWC, Lall K, Liberman MC, Kujawa SG. Aging after noise exposure: Acceleration of cochlear synaptopathy in “recovered” ears. J Neurosci. 2015;35(19):7509-7520.
-
Prendergast G, Guest H, Munro KJ, et al. Effects of noise exposure on young adults with normal audiograms I: Electrophysiology. Hear Res. 2017;344:68-81.
-
Moore DR. Guest editorial: auditory processing disorder. Ear Hear. 2018;39(4) 617–620.
-
Jerger JF. The concept of auditory processing disorder–A brief history. In: Cacace AT, McFarland DJ, eds. Controversies in Central Auditory Processing Disorder. San Diego: Plural Publishing, Inc;2009.
-
Ohio State University. Auditory processing disorders. Available at: https://sphs.osu.edu/clinic/audiology-services/auditory-processing-disorders
-
Kricos PB. Audiologic management of older adults with hearing loss and compromised cognitive/psychoacoustic auditory processing capabilities. Trends Amplif. 2006;10(1):1-28.
-
Moore DR. Sources of pathology underlying listening disorders in children. Intl J Psychophysiol. 2015;95(2):125-134.
-
Beck DL, Clarke JL, Moore DR. Contemporary issues in Auditory Processing Disorders: 2016. Hearing Review. 2016;23(4):22.
-
Beck DL. Super directional hearing aids, noise reduction, and APD: Interview with Harvey Dillon, PhD. Available at: https://www.audiology.org/news/super-directional-hearing-aids-noise-reduction-and-apd-interview-harvey-dillon-phd
-
Keith WJ, Purdy SC. Assistive and therapeutic effects of amplification for Auditory Processing Disorder. Seminars Hear. 2014;35(1):27-38.
-
Starr A, Picton TW, Sininger Y, Hood LJ, Berlin CI. Auditory neuropathy. Brain. 1996;119(3): 741-753.
-
Zeng F-G, Kong Y-Y, Michalewski HJ, Starr A. Perceptual consequences of disrupted auditory nerve activity. J Neurophysiol. 2005;93(6): 3050-3063.
-
Zeng F-G, Liu S. Speech perception in individuals with auditory neuropathy. J Sp Lang Hear Res. 2006;49:367-380.
-
Rance G, Beer DE, Cone-Wesson B, et al. Clinical findings for a group of infants and young children with auditory neuropathy. Ear Hear. 1999;20(3):238-252.
-
Berlin CI, Hood LJ, Morlet T, et al. Multi-site diagnosis and management of 260 patients with Auditory Neuropathy/Dys-synchroncy (Auditory Neuropathy Spectrum disorder). Int J Audiol. 2010;49(1):30-43.
-
Buss E, Labadie RF, Brown CJ, Gross AJ, Grose JH, Pillsbury HC. Outcome of cochlear implantation in pediatric auditory neuropathy. Otol Neurotol. 2002;23(3): 328-332.
-
Teagle HFB, Roush PA, Woodward JS, et al. Cochlear implantation in children with auditory neuropathy spectrum disorder. Ear Hear. 2010;31(3): 325-335.
-
Yuvaraj P, Jayaram M. Audiological profile of adult persons with auditory neuropathy spectrum disorders. J Audiol Otol. 2016;20(3):158-167.
-
Beck DL, Larsen DR, Bush, EJ. Speech in noise: Hearing loss, neurocognitive disorders, aging, traumatic brain injury and more. J Otolaryngol ENT Res. 2018;10(4)199-205.
-
Beck DL. Best practices in hearing aid dispensing: An interview with Michael Valente, PhD. Hearing Review. 2017;24(12):39-41.
-
Clark JG, Huff C, Earl B. Clinical Practice Report Card – Are we meeting best practice standards for adult hearing rehabilitation? Audiology Today. 2017.
-
Bench J, Kowal A, Bamford J. The BKB (Bamford-Kowal-Bench) sentence lists for partially-hearing children. Brit J Audiol. 1979;(3):108-112.
-
BKB-SIN Speech-in-Noise Test. Elk Grove Village, IL: Etymotic Research, Inc.
-
Wilson RH, Carnell CS, Cleghorn AL. The Words-in-Noise (WIN) test with multitalker babble and speech-spectrum noise maskers. J Am Acad Audiol. 2007;18(6):522-529.
-
Nilsson M, Soli SD, Sullivan JA. Development of the Hearing in Noise Test for the measurement of speech reception thresholds in quiet and in noise. J Acoust Soc Am. 1994;95(2):1085.
-
Killion MC, Niquette PA, Gudmundsen GI, Revit LJ, Banerjee S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J Acoust Soc Am. 2004;116(4): 2395-2405.
-
Schafter EC. Speech perception in noise measures for children: A critical review and case studies. J Educ Audiol. 2010;16:4-15.
-
Bench J, Kowal A, Bamford J. The BKB (Bamford-Kowal-Bench) sentence lists for partially-hearing children. Brit J Audiol. 1979;13:108-112.
-
Nilsson MJ, Soli SD, Gelnett DJ. Development of the hearing- in-noise test for children (HINT-C). Los Angeles: House Ear Institute;1992.
-
Jerger S, Jerger J. Pediatric Speech Intelligibility Test: Manual for Administration. St Louis, Mo: Auditec;1984.
-
Spahr AJ, Dorman MF, Litvak LM, et al. Development and validation of the pediatric AzBio sentence lists. Ear Hear. 2014;35(4):418-422.
-
Spahr AJ, Dorman MF, Litvak LM, et al. Development and validation of the AzBio sentence lists. Ear Hear. 2012;33(1):112-117.
-
Cox RM, Alexander GC, Gray GA. Personality, hearing problems, and amplification characteristics: Contributions to self-report hearing aid outcomes. Ear Hear. 2007;28(2):141-162.
-
Kalikow DN, Stevens KN. Development of a test of speech intelligibility in noise using sentence materials with controlled word predictability. Acoust Soc Am. 1977;61(5):1337.
-
Beck DL, Nilsson M. Speech-in-noise testing: Speech-in-noise testing: A pragmatic addendum to hearing aid fittings. Hearing Review. 2013;20(5):24-26.
-
Wilson RH. Clinical experience with the Words-in-Noise test on 3430 veterans: Comparison with pure-tone thresholds and word recognition in quiet. J Am Acad Audiol. 2011;22(7):405-423.
-
Picou EM, Ricketts TA, Hornsby BWY. How hearing aids, background noise, and visual cues influence objective listening effort. Ear Hear. 2013;34(5):e52-e64.
-
McGarrigle R, Munro KJ, Dawes P. Listening effort and fatigue: What exactly are we measuring? A British Society of Audiology Cognition in Hearing Special Interest Group ‘white paper.’ Int J Audiol. 2014;53(7):433-445.
-
Johnson JA, Xu J, Cox, RM. Impact of hearing aid technology on outcomes in daily life II: Speech understanding and listening effort. Ear Hear. 2016;37(5):529-40.
-
Thibodeau LM, Schaper L. Benefits of digital wireless technology for persons with hearing aids. Seminars Hear. 2014;35(3):168-176.
-
Johnston KN, John AB, Kreisman NV, Hall JW, Crandell CC. Multiple benefits of personal FM system use by children with auditory processing disorder (APD). Int J Audiol. 2009;48(6):371-383.
-
Kuk F, Jackson A, Keenan D, Lau C-C. Personal amplification for school-age children with auditory processing disorders. J Am Acad Audiol. 2008;19(6):465-480.
-
DeConde Johnson C, Thibodeau LK, Wolfe J, et al. An overview of wireless technology to improve communication in noise. April 2, 2015. Available at: https://www.audiologyonline.com/audiology-ceus/course/overview-wireless-technology-to-improve-25748
-
Saunders GH, Frederick MT, Chisolm TH, Silverman SP, Arnold M, Myers P. Use of a frequency-modulated system for veterans with blast exposure, perceived hearing problems, and normal hearing sensitivity. Seminars Hear. 2014;35(3):227-238.
-
Gallun FJ, Papesh MA, Lewis MS. Hearing complaints among veterans following traumatic brain injury. Brain Injury. 2017;31(9):1183-1187.
-
Saunders GH, Frederick MT, Arnold ML, Silverman SC, Chisholm TH, Myers PJ. A randomized controlled trial to evaluate approaches to auditory rehabilitation for blast-exposed veterans with normal or near-normal hearing who report hearing problems in difficult listening situations. J Am Acad Audiol. 2018;29(1):44-62.
-
Smart JL, Kelly AS, Searchfield GD, Lyons AM, Houghton JM. Rehabilitation of adults with auditory processing disorder and normal peripheral hearing: Two case studies. Aust N Z J Audiol. 2007;29(1):53-59.
-
Galster JA, Rodemerk KS. The benefit of remote microphones with four different wireless protocols. Canadian Audiologist. 2016;3(2). Available at: http://canadianaudiologist.ca/the-benefit-of-remote-microphones-with-four-different-wireless-protocols-feature/
-
Valente M, Oeding K, Brockmeyer A, Smith S, Kallogjeri D. Differences in word and phoneme recognition in quiet, sentence recognition in noise, and subjective outcomes between manufacturer first-fit and hearing aids programmed to NAL-NL2 using real-ear measures. J Am Acad Audiol. 2018;29(8):706-721.
-
Winchester RA. When Is a hearing aid needed? Maico Audiological Library Series. 1(12):36-39.
-
Bennett CD. Hearing aid use with minimal high-frequency hearing loss. Otolaryngol Head Neck Surg. 1989;100(2):154-157.
-
Beck DL, Le Goff N. Contemporary hearing aid amplification: Issues and outcomes in 2018. J Otolaryngol-ENT Res. 2018;10(1):00303.
-
Mroz M. FM systems for people with hearing loss. February 2018. Available at: https://www.healthyhearing.com/help/assistive-listening-devices/fm-systems
-
Beck DL, Tomasula MD, Sexton J. FM made friendly. August 28, 2006. Available at: : https://www.audiologyonline.com/articles/fm-made-friendly-973
-
Wolfe J, Morais M, Neumann S, et al. Evaluation of speech recognition with personal FM and classroom audio distribution systems. J Educ Audiol. 2013;19:65-79.
-
Thibodeau L. Comparison of speech recognition with adaptive digital and FM remote microphone hearing assistance technology by listeners who use hearing aids. Am J Audiol. 2014;23:201-210.
-
Wolfe J, Morais M, Schafer E, et al. Evaluation of speech recognition of cochlear implant recipients using a personal digital adaptive radio frequency system. Am J Audiol. 2013;24(8):714-724.
-
Wolfe J, Duke M, Schafer E, et al. Evaluation of performance with an adaptive digital remote microphone system and a digital remote microphone audio-streaming accessory system. Am J Audiol. 2015;24:440-450.
-
Wolfe J, Morais M, Schafer E. Improving hearing performance for cochlear implant recipients with use of a digital, wireless, remote-microphone, audio-streaming accessory. Am J Audiol. 2015;26(6):532-539.
-
Wolfe J. Evaluation of modern remote microphone technologies [PDF]. GN ReSound. Available at: shorturl.at/bNP01
-
Schafer EC, Florence S, Anderson C, et al. A critical review of remote-microphone technology for children with normal hearing and auditory differences. J Educ Audiol. 2014;20:1-11.
-
Salehi H, Parsa V, Folkeard P. Electroacoustic assessment of wireless remote microphone systems. Audiol Res. 2018;8(1):204.
-
Fitzpatrick EM, Séguin C, Schramm DR, Armstrong S, Chénier J. The benefits of remote microphone technology for adults with cochlear implants. Ear Hear. 2009;30(5).590-599.
-
Beck DL, Flexer C. Listening is where hearing meets brain…in children and adults. Hearing Review. 2011;18(2):30-35.
-
Clark JG, English KM. Counseling-Infused Audiologic Care. Boston, Mass: Pearson Education; 2014.
-
Roup CM. The impact of minimal to mild sensorineural hearing loss in adults. Perspectives of the ASHA Special Interest Groups. 2016;1(2):SIG 6.
About the Authors:
Douglas L. Beck, AuD, is Executive Director of Academic Sciences at Oticon Inc, Somerset, NJ; Jeffrey L. Danhauer, PhD, is Emeritus Professor of Audiology, University of California Santa Barbara; Harvey B. Abrams, PhD, is Courtesy Professor at the University of South Florida in Tampa; Samuel R. Atcherson, PhD, is Professor and Director of Audiology at the University of Arkansas for Medical Sciences; David K. Brown, PhD, is Professor and Director of the Audiology SIMLab at Pacific University in Hillsboro, Ore; Marshall Chasin, AuD, is Director of Research at Musicians’ Clinics of Canada in Toronto; John Greer Clark, PhD, is Professor and Director of Audiology Education at the University of Cincinnati; Christine De Placido, PhD, is Senior Lecturer at Queen Margaret University in Edinburgh, Scotland; Brent Edwards, PhD, is Director of the National Acoustic Laboratories (NAL) in Macquarie Park, Australia; David A. Fabry, PhD, is Chief Innovation Officer at Starkey Hearing Technologies, Eden Prairie, Minn; Carol Flexer, PhD, is Distinguished Professor, Emeritus, Audiology at The University of Akron in Ohio; Brian Fligor, ScD, is Chief Development Officer at Lantos Technologies Inc in Boston; Gregory Frazer, PhD, AuD, is Director of Audiology at Pacific Hearing and Balance Inc in Los Angeles; Jason A. Galster, PhD, is Director of Clinical Research at Advanced Bionics LLC, in Valencia, Calif; Laura Gifford, AuD, is Senior Regional Sales Manager at Unitron US, and is based in Nashvillle, Tenn; Carole E. Johnson, PhD, AuD, is Professor in the Department of Communication Sciences and Disorders at the University of Oklahoma Health Sciences Center in Oklahoma City; Jane Madell, PhD, is the owner of Pediatric Audiology Consulting in New York City; David R. Moore, PhD, is Professor of Otolaryngology at the University of Cincinnati College of Medicine in Ohio; Ross J. Roeser, PhD, is the Lois and Howard Wolf Professor in Pediatric Audiology at the University of Texas at Dallas; Gabrielle H. Saunders, PhD, is a researcher at the Eriksholm Research Center in Snellersten, Denmark; Grant D. Searchfield, PhD, is Associate Professor at The University of Auckland in New Zealand; Christopher Spankovich, PhD, AuD, MPH, is Associate Professor and Vice Chair of Research at the University of Mississippi Medical Center in Jackson, Miss; Michael Valente, PhD, is Professor of Clinical Otolaryngology at Washington University in St Louis, Mo; and Jace Wolfe, PhD, is Director of Audiology and Research at Hearts for Hearing in Oklahoma City, Okla.
Correspondence can be addressed to Dr Beck at: [email protected]
Citation for this article: Beck DL, Danhauer JL, Abrams HB, Atcherson SR, Brown DK, Chasin M, Clark JG, De Placido C, Edwards B, Fabry DA, Flexer C, Fligor B, Frazer G, Galster JA, Gifford L, Johnson CE, Madell J, Moore DR, Roeser RJ, Saunders GH, Searchfield GD, Spankovich C, Valente M, Wolfe J. Audiologic considerations for people with normal hearing sensitivity yet hearing difficulty and/or speech-in-noise problems. Hearing Review. 2018;25(10)[Oct]:28-38.





All audiologists should have access to equipment that can test up to at least 16kHz. It’s ridiculous that frequencies aren’t tested beyond 8kHz and the “professionals” throw up their hands and exclaim “i unno lol”.
Technology and methods have improved and if cheap MP3 players from the past can play up to 20kHz, why can’t multi-thousand dollar audiometers do so?
Good job putting together this important article. Windmill and Freeman have been analyzing a decade of data from CMS which is revealing that audiologists are not consistently following ‘best practices’ and looking for the ‘hidden hearing loss’ discussed in this paper. Of the 1.33m Medicare patients evaluated in 2017 by audiologists with pure tone examinations, only 62% had tympanometry and an additional 18% had tymps and reflexes, and about 13% were evaluated with OAEs—never mind exams for tinnitus or vestibular disorders. This article supports the notion that audiologists need to follow best practices as defined and published several years ago by AAA/ASHA/VA and need to go beyond the pure tone examination if they want to properly diagnose, manage, treat patients.
Barry,
But CMS still feels that tympanometry is over used and does not not pay (hospital settings) for it when billed together with 92557.